When Do I Start Annual Breast Imaging?
I find every time I have a speaking engagement, one of the most common questions from the audience is “When do I have to start getting annual breast imaging?” A close second is “How often do I have to get my breast imaging done?” These are excellent questions and if you ask any two physicians, they most certainly will give you a different answer. Almost every professional medical organization has a consensus statement regarding the best time to obtain annual breast imaging.
The general consensus from the American College of Surgeons, American College of Obstetrics and Gynecology, and American College of Radiology, and what I personally practice, is that every average-risk woman should begin breast imaging at the age of 40. She should continue breast imaging annually up until the age of approximately 75. After that point, an imaging schedule should be agreed upon between the patient and the ordering physician.
There is not as much agreement regarding how often a patient should have breast imaging performed (annual vs. biannual). Two of the major concerns with annual breast imaging are: (1) over-diagnosis of breast cancer (specifically, non-invasive breast cancer) that may have never posed a risk to the patient and (2) the need for additional imaging and/or biopsies. Having taken care of breast cancer patients for years, unfortunately, I have seen breast cancers develop in the time between annual mammograms. Therefore, I recommend (and the medical organizations I mentioned above also endorse) yearly mammograms.
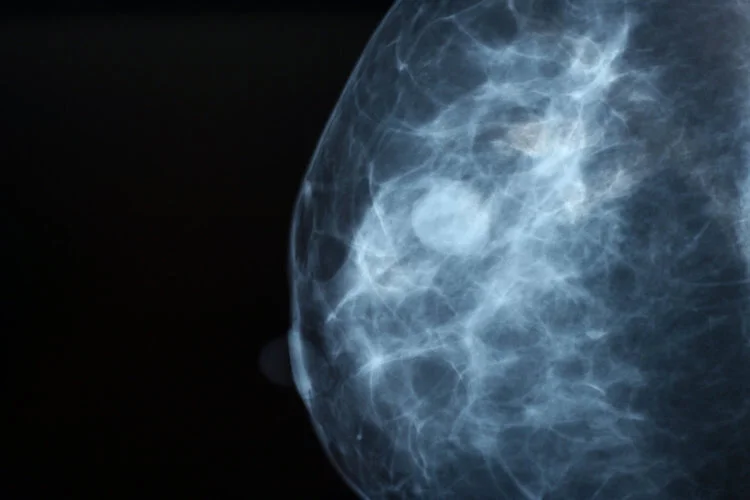
Our breast imaging has improved drastically, even over the last 10 years. A life saved is never an over-diagnosis! Mammograms are able to identify breast cancers up to two years before the patient is able to feel it and this represents an excellent intervention point. Early detection is the key to cure. Non-invasive cancer usually does not form a mass, but is still cancer and warrants appropriate treatment as well. And with the improvement of our imaging and the advent of the 3-D mammogram, we have drastically decreased patient callbacks and unnecessary biopsies.
As with all things, there are exceptions to the rule. Here are a few:
· High-risk patients. These patients usually have a strong family history of breast cancer. Patients considered high risk should begin imaging approximately 10 years before the affected family member was diagnosed with breast cancer (e.g. If your mother was diagnosed with breast cancer at 45 years of age, the patient should begin screening at 35 years of age).
· Genetic mutation carriers. The most common genetic mutation that drastically increases one’s risk of breast cancer is the BRCA genetic mutation. These patients usually begin screening at 25 years of age and have imaging performed every six months. Breast imaging usually alternates between mammogram + ultrasound and bilateral breast MRI. While it has been shown to be safe to monitor patients with genetic mutations closely with imaging, the overwhelming majority of patients opt for bilateral risk-reducing mastectomies.
· “Probably benign” findings. In these cases, the radiologist that reviewed your imaging may identify a finding that they would like to follow closely. For example, a mass that has generally favorable characteristics (such as a cyst) and appears benign or borderline normal calcifications. If your imaging report says that the findings are probably benign, then short-term follow up imaging may be recommended and usually occurs every six months for one to two years.
· Recent benign biopsy. If a patient has needed a biopsy for a concerning finding on imaging, s/he will usually require short-term follow-up imaging (usually at the six-month mark) to confirm stability of the area in question.
· Personal history of breast cancer. If a woman has alreadybeen diagnosed with and treated for breast cancer, she usually needs dedicated breast imaging of the affected breast every 6 months post-treatment for a minimum of two years to confirm stability after surgery and/or treatment.
While life often gets in the way of self-care, please remember to schedule all of your regular screenings, such as a mammogram, colonoscopy, eye exams, and general wellness exams. Prevention is always cheaper than treatment!
If you have any additional questions regarding this information, please contact us.
With love,
Disclaimer: This article is not a substitution for seeking medical attention